
Should Doctors Attend To Patients With ‘Do Not Resuscitate Tattoos’?

Doctors at the University of Miami hospital were confronted with a dilemma when a 70-year-old unconscious man with a tattoo “do not resuscitate” boldly written on his chest was wheeled in by hospital attendants.
This incident as shocking as it is has sparked no little controversy between doctors and ethicists. The debate is on whether the dying man should be saved, or to honor the choice of a supposedly rational human capable of taking actions to which he is solely responsible for.
The 70-year-old man, who was intoxicated probably with alcohol had a long-standing history of heart and lung diseases. All efforts that were directed towards reaching out to his family proved abortive owing to his elevated blood-alcohol level.
His pulse was quite unstable, and in a bid to revive him, doctors made frantic efforts to save him but were unable to salvage the situation as he passed on. Paramedics wheeled the victim into the hospital emergency after finding him unconscious on the street.
After so much deliberation between ethicists and doctors, a deal was struck to respect the man’s tattoo. The dilemma helped them realize the need for an updated system of getting to know patient’s end of life wishes.
Dr. Greg Holt, one of the doctors at Miami hospital who attempted to the patient, asserted the fact that the man’s tattoo appeared to be a unique one which drew not only his attention but also the attention of his colleagues.
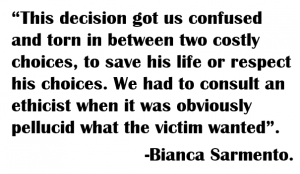
Another doctor available at the scene was Bianca Sarmento, explained that they decided to honor the victim’s tattoo as it entailed the unavoidable principle of not choosing an irreversible path when faced with uncertainty.
After going through his medical history, ethics consultants explained to the doctors the reason why the order on the victim’s tattoo had to be followed strictly.
It was suggested that it sounded more rational and reasonable to admit that the tattoo connoted an implied choice, which served as a caution and also an obligation to a ceremony to which the patient would gladly like to adhere to. Intuitively, the law is sometimes not supposed to interfere with patient-centered care and respect for the best interests of patients in this situation.
The doctors put a halt to the treatment they were administering on the patient. The major object of concern for them was that the tattoo did not serve as a legally binding contract like an originally signed, Do Not Resuscitate Order.
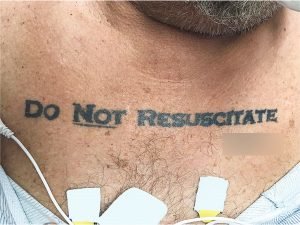
70-year-old-man with a DNR tattoo
The do not resuscitate tattoo had an emphasis on the not to cause no need for further confusion or dilemma.
Dr. Greg stated that his team’s major concern was legality and lawfulness.
Tattoos are not meant to be legally binding do not resuscitate orders. There are quite a good number of requirements for legal orders in Florida. For any DNR order to hold, there needs to be a compromise between the doctor and patient and this involves not only oral dialogue but the participation of trusted signatories.
Medical privacy laws protect every DNR order. People who want DNRs have to go through a regimented process of filling out standard forms and documents with trusted doctors. They get bracelets or wallets cards which state their statuses.
In another interesting case study, doctors discovered a tattoo with a DNR inscription on the leg of a man awaiting amputation. When confronted with this the man opined that it was the opposite of his wishes.
The supposed patient, a hospital worker, had lost a bet which he staked when he was younger, and then agreed to a tattoo but never thought anyone would take his tattoo seriously.

DNRs are equivalent to euthanasia, a situation in which patient desires to die in the face of a possible medical attention owing to the distress caused by the ailment, he/she is suffering from.
It could be either active or passive. It is passive when the patient’s kin agrees to put an end to the patient’s life because of financial implications of the ailment or their feeling of pity they experience when they keep on seeding the patient in that condition. Most times this is done without the patient’s consent.
It becomes active when the ailing patient willingly consents to have his life exterminated by the doctor through injections or tablets.
It is necessary that a person’s choices should be considered, regarded and honored as long as it has to do with conscious, reasonable and rational obligations.
More in Medical Conditions
-
A Comprehensive Guide on How to Heal Anxious Attachment Style
If you often find yourself seeking constant reassurance from your partner or requiring endless validation to feel secure, you may be...
June 1, 2024 -
Why Is My Skin Peeling on My Face After Skincare? Here’s What You Need to Know
Experiencing skin peeling on your face after implementing a skincare routine can be perplexing and frustrating. This phenomenon, where the skin...
May 23, 2024 -
What Is a Mental Edge, and How Do You Get It?
Have you ever wondered why some individuals seem unshakably confident under intense pressure, finding a way to excel when it matters...
May 15, 2024 -
When to Worry About Varicose Veins? Here’s What You Need to Know
Varicose veins are a common issue, affecting about 20% of adults. They’re usually seen as unsightly blemishes on the legs but...
May 12, 2024 -
Why Is Discipline Important: The Ultimate Guide to the Importance of Discipline
Discipline is undoubtedly one of life’s most crucial character traits. It shapes how we approach tasks, manage our time, and...
May 3, 2024 -
Have I Fallen Out of Love or Am I Depressed? Everything You Need to Know
Have I fallen out of love or am I depressed? You’re not alone in this query. In the diversity of human...
April 26, 2024 -
What Does Lung Cancer Breath Smell Like?
Cancer is one of the most formidable diseases of our time, characterized by the uncontrolled growth of cells that invade and...
April 20, 2024 -
Making Major Life Changes? Discover 5 Crucial Things Before You Leap
Life changes are a pivotal part of our journey, marking the transition from one phase of life to another. These changes,...
April 13, 2024 -
The Surprising Benefits of Being Bored at Work
Are you bored at work? We’ve all been there, staring blankly at our computer screens, feeling an overwhelming urge to be...
April 6, 2024















You must be logged in to post a comment Login